High Eye Pressure: What It Is, Causes, & Glaucoma Risk
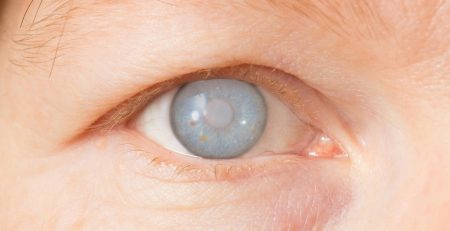
A routine eye check can sometimes flag high eye pressure, medically known as ocular hypertension, a key risk factor for glaucoma. Glaucoma is a serious disease that silently damages the optic nerve, leading to irreversible vision loss.
Understanding this risk is the crucial first step toward protecting your future sight, and seeking expert care is your best defense against this “silent thief.”
Understanding High Eye Pressure: A Silent Threat to Your Vision
High eye pressure is the primary factor that specialists like Dr. Roy Tan monitor, as a sustained elevation can cause the slow, permanent damage characteristic of glaucoma. It is crucial to understand the difference between simply having elevated pressure and the disease itself.
What is High Eye Pressure (Ocular Hypertension)?
High eye pressure occurs when the pressure inside the eye, or Intraocular Pressure (IOP), is consistently elevated above the statistically normal range. The IOP is the balance of fluid production and drainage within the eye’s front chamber.

- Definition: Ocular Hypertension is the term used when a patient has a persistently high eye pressure reading but no detectable damage to the optic nerve or loss of visual field.
- The “Normal Range”: Eye pressure is measured in millimetres of mercury (mmHg). While this can vary, an IOP reading greater than 21 mmHg is typically considered high and warrants close monitoring or intervention.
- Crucial Difference: High Eye Pressure vs. Glaucoma: The distinction is vital. High eye pressure is a risk factor, while glaucoma is the disease itself, optic nerve damage caused by this pressure. Not everyone with elevated IOP develops glaucoma, but nearly every person with glaucoma has, or has had, high eye pressure.
Why High Eye Pressure Is Often Undetected
One of the most concerning aspects of ocular hypertension and early glaucoma is the lack of noticeable symptoms, which is why it is tragically dubbed the “silent thief of sight.”
- Can you feel high eye pressure? In most cases of chronic, open-angle high eye pressure, the answer is a resounding no. Elevated IOP does not cause pain or blurred vision in its initial stages because the pressure rise is gradual.
- What is considered dangerously high eye pressure? While an IOP of 22 mmHg is generally the threshold for diagnosis, what is truly ‘dangerous’ is the effect of sustained pressure on your unique optic nerve. For some, pressure consistently in the upper twenties may rapidly lead to damage, while others may tolerate it better. The danger lies in the lack of screening and the resultant focus on the sustained elevated pressure that, over time, damages the fragile bundle of nerve fibres connecting the eye to the brain. Once those fibres are lost, they cannot be regenerated, leading to permanent blind spots.
The Root Causes of High Eye Pressure & Risk Factors
Understanding the mechanical and biological reasons behind high eye pressure is key to appreciating why regular eye screenings are an essential health necessity in Singapore. The cause is generally related to the plumbing system of the eye, which can be affected by both structural problems and inherent risk factors.
The Science: How Aqueous Humour Imbalance Leads to High IOP
The main reason why eye pressure is high stems from a mechanical problem with the aqueous humour fluid.
- Overproduction of Aqueous Humour: While less common, the ciliary body (the tissue that produces the fluid) can produce too much aqueous humour for the drainage system to handle, leading to an increase in IOP.
- Blocked Drainage (Trabecular Meshwork): This is the most common internal factor. The trabecular meshwork is a spongy filter located in the angle between the iris and the cornea. If this meshwork is clogged (in Primary Open-Angle Glaucoma) or physically blocked (in Primary Angle-Closure Glaucoma, which is common in Asians), the fluid backs up, causing high eye pressure.
- Internal factors such as the structure of the iris and cornea, or inflammation following injury or surgery, can also impede drainage.
Who is at Risk? Key High-Risk Factors
Certain groups face elevated chances of developing high eye pressure and glaucoma:
- Age: Risk increases substantially after age 40, with prevalence continuing to rise with each passing decade
- Family history: Having a parent or sibling with glaucoma or ocular hypertension raises your risk by 4-9 times
- Diabetes: Fluctuating blood sugar levels can affect aqueous humour dynamics and drainage efficiency
- High blood pressure: Hypertension may contribute to impaired ocular blood flow and nerve damage
- Extreme refractive errors: Severe myopia (short-sightedness) or hyperopia (long-sightedness) alters eye structure and drainage
- Prolonged corticosteroid use: Steroid medications, whether eye drops, tablets, inhalers, or creams, can elevate eye pressure
- Previous eye injury or surgery: Trauma or surgical complications may damage drainage structures permanently
Diagnosis: Measuring Your Intraocular Pressure (IOP)

The diagnosis of high eye pressure and glaucoma relies on a combination of specific measurements and tests. Identifying the problem early is paramount, as detection provides the opportunity to prevent further loss of sight.
The Only Way to Know: The Comprehensive Eye Exam
A specialist eye exam goes beyond a standard vision test to look deep into the health of the eye’s internal structures.
- Diagnosis: The IOP is measured using an instrument called a tonometer. This instrument uses a tiny, flat-tipped device that gently touches the surface of the eye to measure the resistance. This is a quick and painless procedure that definitively answers the question of what eye pressure is too high.
- Other Essential Tests: Because glaucoma is a disease of the optic nerve, an IOP reading alone is not enough. Your specialist will conduct a comprehensive battery of tests:
- Ophthalmoscopy: Checking the optic nerve for structural damage (cupping) caused by the pressure.
- Pachymetry: Measuring the Central Corneal Thickness (CCT), as this influences the accuracy of the IOP reading.
- Visual Field Tests (Perimetry): Mapping your peripheral and central vision to detect early, subtle blind spots.
- Gonioscopy: Examining the eye’s drainage angle to classify the type of glaucoma (open-angle or angle-closure).
- Ophthalmoscopy: Checking the optic nerve for structural damage (cupping) caused by the pressure.
Is Eye Pressure of 22 High? What Your Numbers Mean
Understanding your IOP reading helps you appreciate the need for specialist care. The numeric value provides the baseline for all subsequent monitoring and treatment decisions.
- Interpreting Results: IOP is considered to be in the normal range between 10–21 mmHg. An IOP reading of 22 mmHg or higher puts you in the ocular hypertension category. While is eye pressure of 22 high, it is the combination of this number, your optic nerve appearance, and other risk factors (like family history or thin corneas) that determines your true risk of developing glaucoma.
- The Follow-Up: For patients with high eye pressure but no optic nerve damage, the typical recommendation is close monitoring. This involves regular comprehensive eye exams to track your pressure levels and to ensure no nerve damage develops. However, if your pressure is extremely elevated, or if you have multiple risk factors, your specialist may recommend immediate treatment to lower your IOP and protect your vision.
Effective Management and Treatment Options to Lower Eye Pressure
For patients diagnosed with high eye pressure that poses a high risk, or those already showing signs of glaucoma damage, treatment becomes a priority. The primary goal of all glaucoma treatment is to lower the IOP to a safe or “target” pressure, thereby stopping the progression of optic nerve damage.
Prescription Medications: The First Line of Defence
Eye drops are the most common initial treatment for controlling high eye pressure. They are effective, non-invasive, and work by improving the balance of aqueous humour fluid.
- Eye Drops: How They Work: These prescription drops generally fall into two categories:
- Decrease Fluid Production: They reduce the rate at which the eye produces aqueous humour, thus reducing the total volume and lowering pressure.
- Increase Fluid Drainage: They help the trabecular meshwork work more efficiently to drain the aqueous humour away from the eye.
- Decrease Fluid Production: They reduce the rate at which the eye produces aqueous humour, thus reducing the total volume and lowering pressure.
- Focus on Compliance: The effectiveness of this treatment hinges entirely on using the drops exactly as prescribed. Failing to adhere to the schedule can lead to significant pressure spikes, resulting in a loss of vision. If you struggle with the routine, speak to Dr. Tan about strategies or alternative therapies.
Procedures and Surgery: When Drops Aren’t Enough
If medication fails to bring the IOP down to the target pressure, or if the glaucoma is progressive despite drops, Dr. Tan may recommend an in-clinic procedure or surgery to improve the eye’s natural drainage system.
- Laser Therapy (e.g., SLT/ALT): Selective Laser Trabeculoplasty (SLT) is a common, non-invasive treatment often performed in the clinic. It uses a low-power laser to treat the drainage angle, prompting the tissue to work more efficiently and improve outflow, which effectively answers how you treat high eye pressure when drops are inadequate.
- Traditional Surgery: As a trusted eye surgeon, Dr. Tan is qualified to perform more intricate surgical procedures when necessary.
- Minimally Invasive Glaucoma Surgery (MIGS): These newer, less-invasive surgeries are often done in conjunction with cataract surgery and involve implanting microscopic devices to improve drainage.
Lifestyle Adjustments: Supporting Your Eyes Naturally
While no lifestyle change can substitute for medical or surgical treatment, certain adjustments can help support your overall eye health and assist in the management of high eye pressure. These are complementary steps that work in tandem with your specialist-prescribed regimen.
The Role of Diet and Exercise in Eye Health
A well-rounded, healthy lifestyle has indirect but positive benefits for your systemic health, which in turn can influence your IOP.
- Diet: Focus on a balanced diet rich in antioxidants. Foods high in Omega-3 fatty acids (like oily fish) and leafy greens (which contain nitrates) are thought to promote healthy blood flow to the optic nerve.
- Exercise: Regular, moderate aerobic exercise (like walking or cycling) has been shown to temporarily lower IOP in some patients. It is important, however, to be mindful of certain activities. If you are diagnosed with advanced glaucoma or have a very high eye pressure reading, you should limit high-intensity activities that involve prolonged head-down positions (like certain yoga poses or heavy weightlifting), as these can momentarily increase pressure.
Managing Stress and Caffeine Intake
External factors that influence systemic blood pressure and internal anxiety can also have a subtle effect on your eye health.
- Managing Stress and Caffeine Intake: Chronic, unmanaged stress can elevate your overall blood pressure, which may indirectly affect ocular health. Finding healthy ways to manage stress, such as mindfulness or spending time in nature, is beneficial.
- How to lower eye pressure fast at home? It is vital to maintain realistic expectations: no home remedy or lifestyle change can substitute for medical drops, lasers, or surgery recommended by a specialist. These adjustments are supportive measures, not curative ones. If you suspect your eye pressure is rapidly rising (e.g., in an acute angle-closure attack), you must seek immediate emergency medical attention, not rely on home remedies.
Why Choose Dr Roy Tan at Cornerstone Eye Centre, Novena
Dr Roy Tan brings extensive expertise in glaucoma management to patients at Cornerstone Eye Centre in Novena. As a glaucoma specialist, Dr Tan offers comprehensive care from diagnosis through surgical intervention, including minimally invasive techniques.
Cornerstone Eye Centre provides:
- Range of diagnostic equipment for precise glaucoma assessment
- Full spectrum of treatment options, from medications to MIGS and conventional surgery
- Personalised treatment plans tailored to your specific condition and lifestyle
- Convenient Novena location with modern facilities
- Dedicated follow-up care to monitor treatment effectiveness
Early detection and proper management are paramount in preserving your vision. If you’re concerned about glaucoma or seeking a second opinion on your current treatment plan, Dr Tan and his team are ready to help you navigate your options.
Take the Next Step
Early detection and treatment are crucial to safeguarding your vision from the irreversible damage caused by glaucoma.
Book the Comprehensive $88 Cataract & Glaucoma Screening.
Book a Cataract & Glaucoma Screening for $88
Don’t wait for symptoms to appear before taking action. Early detection is key to preserving your vision.
At Dr Roy Tan’s clinic, we offer a comprehensive Cataract & Glaucoma Screening for just $88. This screening is designed to assess your eye health thoroughly, identify any early indicators of glaucoma or cataracts, and discuss your personalised options if either condition is detected.